About Us
What do you want to know ?
Agnus Group Healthcare Services is committed to offering value added healthcare revenue cycle management solutions to clients for performance optimization and to boost profitability. We have always aimed to be value partners to our clients, taking pride in their business growth. The need for medical billing and coding outsourcing companies like us is increasing due to our comprehensive, sustainable and scalable medical billing and coding services and experienced resources.
Medical audits involve the systematic review of clinical documents, coding, billing records, and claims to ensure accuracy, compliance, and optimal revenue. Audits can be conducted internally by the healthcare provider or externally by third parties or regulatory bodies.
Our company Services
Payment Posting
the process of recording payments from insurance companies, patients, and other payers to a patient’s account in the billing system. Payment posting is a critical step in managing and closing the billing cycle, as it allows healthcare providers to track revenue, identify issues with claims, and ensure that payments match the expected reimbursement amounts,Receiving Payments,Reviewing EOBs and ERAs etc
Go to deatils...Hospitals treatment
Hospital treatment encompasses a wide range of medical services provided to patients in a hospital setting. These treatments can vary from emergency care to complex surgical procedures, and from short-term acute care to long-term management of chronic conditions. Hospitals are equipped with specialized medical professionals, advanced technology, and facilities designed to provide comprehensive care to patients. like Emergency Care ,Inpatient Care
Go to deatils...Physician Groups
Physician groups, also known as medical groups or physician practices, are organizations or networks of doctors who come together to provide services.These groups can vary in size and structure, ranging from small practices with a few physicians to large, multispecialty groups with hundreds of doctors.Physician groups play a crucial role in delivering coordinated, comprehensive care to patients across various specialties.like Specialty Group,Multispecialty...
Go to deatils...Pre-Authorization Analyst
A Pre-Authorization Analyst, also known as a Pre-Auth Analyst or Prior Authorization Specialist, plays a crucial role in healthcare administration by ensuring that medical procedures, services, or prescriptions are pre-approved by insurance companies before they are carried out.Pre-Authorization Analysts play a vital role in preventing claim denials and ensuring smooth reimbursement processes, which directly impacts the financial health of healthcare providers. they help reduce the risk of claims being rejected or delayed due to lack of approval
Go to deatils...AR Denial Management
AR Denial Management refers to the process of managing, investigating, and appealing denied insurance claims in healthcare. It is a critical part of the Accounts Receivable (AR) management and Revenue Cycle Management (RCM) process, focusing on addressing claims that have been rejected or denied by payers (insurance companies) for various reasons. denial management helps healthcare providers recover revenue that would otherwise be lost, ensuring timely payments and improving the organization's financial health.
Go to deatils...Quality Analyst
A Quality Analyst (QA) in the Healthcare Revenue Cycle Management (RCM) field is responsible for ensuring the accuracy, compliance, and overall quality of processes involved in managing the financial transactions of healthcare organizations. This includes tasks related to claims submission, coding, billing, payment posting, and denial management. The QA's role is crucial in maintaining high standards of performance, reducing errors, and ensuring that the organization follows industry regulations and payer requirements.
Go to deatils...Our Team Leadership

Ankit Gour
SVP of Marketing
Ankit Gour is a seasoned marketing executive with over 5+ years of experience in driving business growth through strategic marketing initiatives...
More Details
Abhishek Dave
Co-Founder & Chief Executive Officer
Abhishek Dave is a Agnus Group entrepreneur and healthcare industry expert with over 6 years of experience in driving innovation and growth...
More Details
Aryan Kaur
SVP of HR & Compliance
Aryan Kaur is a seasoned HR and compliance expert with over 5+ years of experience in driving organizational growth and ensuring regulatory adherence. As SVP of HR & Compliance...
More DetailsGet in touch
Contact Information
-
3rd floor, Saptagiri Towers, 301, Mayur Marg,
Begumpet, Hyderabad, Telangana-500016. -
hr@agnusgrouphealthcareservices.com
-
info@agnusgrouphealthcareservices.com
What our clients have to say about us

Agnus Group Healthcare Services has been an outstanding partner. They seamlessly transitioned their workforce to work from home to meet our operational needs during a time of uncertainty. Their support has enabled us to maintain productivity and client satisfaction during this challenging time.
Alexis Atkins
HR Manager
Our company has a long-standing partnership with Agnus Group Healthcare Services and were very pleased with their proactive action when shifting to a work from home environment. We have not seen any loss in production during this period of time.
Aakriti Menon
Senior Director of Services
Agnus Group Healthcare Services is not just our vendor but rather has been an integral part of the success story of our company and we are delighted with this partnership and intend to continue to grow our business with our preferred partner in the years to come. Our progressive increase in Coding accuracy is a direct result of the accurate and professional services provided by Agnus Group Healthcare Services.
Aarav Dhillon
Senior Assistant Manager
The timelines and chronologies are customized according to the guidelines provided. Great job! The analytical and logical summaries from Agnus Group Healthcare Services exceed my expectations as a QME. Good job Team.
Akash Jain
Assistant ManagerFrequently Asked Questions
Latest Blog & News

The Importance of Accurate Medical Coding in Revenue Cycle Management
Accurate medical coding is a cornerstone of effective revenue cycle management (RCM) in healthcare organizations. It involves translating medical diagnoses, procedures, and services into standardized codes used for billing and insurance claims...
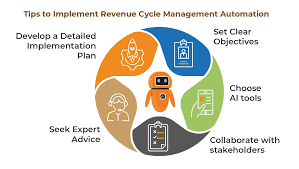
What Is Revenue Cycle Management Automation
An automated revenue cycle can help optimize your healthcare organization’s entire workflow, driving revenue and boosting your competitive advantage. But what is healthcare revenue cycle management automation and how can it work for you? Intelligent automation (IA) involves robotic process automation (RPA) ...

AI in Revenue Cycle Management: How It Improves RCM, Efficiency and Revenue
Artificial Intelligence has the potential to significantly impact the field of Revenue Cycle Management in the US healthcare industry. This article explores how to implement AI in RCM, overcome obstacles...